Are life’s endless menus exhausting you? Escape the burdens of the ‘axiom of choice’
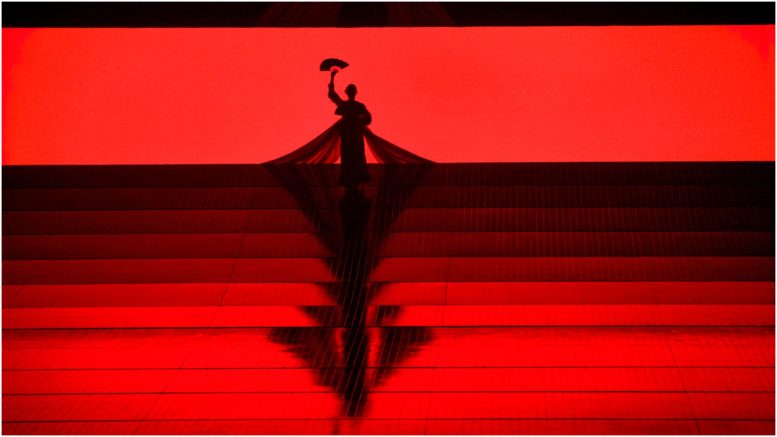
ILLUSTRATION: TOMASZ WALENTA
Sometimes I stare at a restaurant menu with no idea how to choose my dinner. It might be because the menu has too many appealing options, but often it’s because I have decision fatigue. This is when you make too many decisions in one day and then find it hard to make any more. It doesn’t matter how important those decisions are. It could be deciding what shoes to wear or whether to buy a house. Each decision takes a toll.
There is a piece of mathematics dealing with this problem called the axiom of choice. It holds that, given any collection of sets, with each one containing at least one object, it is possible to select exactly one object from each set—even if the collection of sets is infinite. The axiom of choice asserts, in other words, that we can make an infinite number of individual choices.
In mathematics, an axiom is a basic truth that we assume without proof. In fact, we can’t prove it. If we could prove it, it would be called a theorem. Although mathematics is all about proving things with rigorous logic, we have to start with some assumptions because it is not possible to prove anything from nothing.
The axiom of choice can be expressed in terms of what mathematicians call a choice function. Given a collection of choices from, say, an infinite set of restaurant menus, a choice function selects one meal from each. Because menus are so varied, however, that could be quite a burden of choice!
Some choice functions, however, can let us escape the axiom of choice—by making an infinite number of choices unnecessary. Faced with an infinite number of menus, our choice function could be: “Always pick the least expensive item” or “Always pick the least caloric.” We would make one global choice and repeat it infinitely instead of making an infinite number of individual choices.
The same holds for simpler choices, but as with the menus, our ability to escape the axiom of choice depends on the sort of objects we are choosing. Consider the difference, in terms of organizing your closet, between sets that consist of pairs of socks or pairs of shoes. For the socks, you have to choose which of the pair to tidy first (assuming the socks have no features distinguishing left from right). With the shoes, you can just make one choice at the start: to put away, say, the left shoe first every time. Again, you’re able to make the same choice an infinite number of times.
In mathematics as in real life, dealing with the prospect of infinite choices is daunting, but we can avoid it by making one global choice instead. The problems arise when the choices can’t be easily ranked or when they’re not distinguishable from one another.
Another way to define a choice function that escapes the burden of infinite choices is to use an algorithm. This doesn’t make one global choice but instead provides a scheme for choosing, without your having to make any decisions along the way. For example, I could choose to walk the same route to work every day, or I could use an algorithm that says I will take the most direct route in the city grid until I hit a red light at a crosswalk, at which point I will turn and take the most direct route from my new position. The first way removes all choices but might be boring; the second provides some variation but without my having to make any decisions.
The axiom of choice is a powerful tool, but efficient mathematicians prefer to avoid using it where possible, saving it only for problems where it’s really necessary. We can likewise avoid decision fatigue in daily life by using global choices or algorithms, thus saving our decision-making energy for more important choices.




 Article Info
Article Info