Tuesday, May 31, 2011
NHS & Kaiser Permanente: Can we still learn?
It is amazing how planners often overlook the most important aspect of why an organisation such as Kaiser Permanente is a success. Having looked at some of their ways of saving money in my last post, I need now look at why Kaiser Permanente is such a success. New York Times
What perhaps the NHS should not ignore is one very important but simple way to contain cost: salaries for doctors, not fees.
The current thinking of containing cost in the NHS by limits set to GP Commissioning will end up in many patients not getting the essential treatments they need and GPs being blamed for poor commissioning.
Foundation Trusts will be expected to balance books or make a profit. Instead of controlling unnecessary investigation and treatment Trusts would need to treat more patients. This is not the thinking behind Kaiser Permanente and is indeed the opposite to their philosophy. It may well be fine to make money from rich overseas patients, but there is a limit as to the availability of specialist time. Ultimately NHS patients will suffer.
The side effect of the current drive of GP Commissioning is that it would no longer matter if Foundation Trusts are private or not. Before long most specialists would only offer their expert services via private organisations. Why else are the Private Health Organisations hovering around!!!
The side effect of the current drive of GP Commissioning is that it would no longer matter if Foundation Trusts are private or not. Before long most specialists would only offer their expert services via private organisations. Why else are the Private Health Organisations hovering around!!!
What can GP Commissioners do?
Do exactly what Kaiser Permanente is doing: integrate!!! Integrate primary and specialist care. Pay doctors at both levels salaries, not fees! In fact both the Mayo Clinic and the Cleveland Clinic pay their doctors salaries as well as the VA and a number of other hospitals including Johns Hopkins.
Yes, employ the specialists; buy up the hospitals and buy back pathology and other services.
Not big enough: join up with other commissioners.
What about very special services such as those provided by Royal Marsden, Queens Square, Papworth & GOS?
This can be similar to Kaiser’s arrangement with UC for kidney transplants.
But this is like the old days of Regional Health Authorities!!!
Right, did you not notice that the old black lace is back in fashion: the old black is the new black!!!
NHS-Kaiser Permanente: Summary Posts
I might as well include all the Kaiser Permanente posts:
Dec 22, 2010
Ownership and integration has undoubtedly been the hallmark of Kaiser Permanente and many observers believe that this is the main reason for its success, not so much the offering of choice to its members. Yes, members, as Kaiser Permanente is very much a Health Club, rather than an Insurer. Also, a not so well known fact is that Kaiser doctors are not allowed to practise outside the system.
It is evident that the drive to offer so called choice in the NHS, and the ensuing cross-billing, has pushed up cost
When Hospital Trusts are squeezed, true choice is no longer there. Kaiser Permanente members in fact sacrifice choice for a better value health (and life style) programme.
Jan 02, 2011
Look at major hospitals in England: Urgent Care Centres are set up and staffed by nurse practitioner, emergency nurse practitioners and GPs so that the charge by the Hospital Trusts (soon to be Foundation Trusts) for some people who tried to attend A & E could be avoided. It is often a time wasting exercise and many patients still need to be referred to the “real” A & E thus wasting much valuable time for the critically ill patients and provided fodder for the tabloid press. And payment still had to be made. Currently it is around £77.00 a go. But wait for this, over the New Year some of these Centres would employ off duty A & E Juniors to work there to save some money that Trusts could have charged.
This is certainly not how Kaiser Permanente would run things: all integrated and no such thing as “cross charging”. In fact the doctors are not on a fee-for-service basis but like Mayo Clinic, Cleveland Clinic and Johns Hopkins Hospital, doctors are paid a salary.
Feb 23, 2011
Kaiser Permanente does not cover everybody and by being able to reject or remove the chronically ill the comparison with the NHS was at best meaningless and at worst ……well I do not really want to say.
So what would they do by 2014 when they can no longer reject pre-existing conditions.
Well, their founding fathers may well have ensured their ability to continue.
Kaiser Permanent is not a Health Insurer, it is in fact a Health Maintenance Organisation. I have no doubt in my mind that they will if need be just become a Health Maintenance Club with services by amongst others, integrated primary care and secondary care doctors.
Mar 02, 2011
From one of their own advisers: Prof Chris Ham
Chris Ham"May I add something briefly? The big question is not whether GP commissioners need expert advice or patient input or other sources of information. The big problem that we have had over the past 20 years, in successive attempts to apply market principles in the NHS, has been the fundamental weakness of commissioning, whether done by managers or GPs, and whether it has been fundholding or total purchasing."
“………The barriers include government policies that risk further fragmenting care rather than supporting closer integration. Particularly important in this respect are NHS Foundation Trusts based on acute hospitals only, the system of payment by results that rewards additional hospital activity, and practice based commissioning that, in the wrong hands, could accentuate instead of reduce divisions between primary and secondary care.”
Saturday, May 28, 2011
NHS Reform: Space, Snorkel & Scotland
Sometimes in life the solution to a big problem could be so simple.
Now that David Cameron and Andrew Lansley are faced with major delays in the proposed NHS reform, the Cockroach Catcher may have a simple solution for them.
Remember the very old Urban Myth about NASA spending millions on developing a zero gravity pen:
The Myth did get into one episode of The West Wing: We Killed Yamamoto
Leo: We spent millions of dollars developing a pen for the astronauts that would work in zero gravity. Know what the Russians did?
Toby: Used a pencil?
Leo: They used a pencil.
Toby: Used a pencil?
Leo: They used a pencil.
Well it was not exactly true but it illustrated a very important point: solutions could sometimes be very simple and cheap.
Now most readers know that I love snorkeling and when I started my wife on it she, being a scientist, wanted to know the names of things she saw whilst snorkeling. The West Wing came to mind.
We used a polypropylene chopping board (the smaller one), drill a hole in the corner to tie a strap so that the hand could sometimes be free to operate the camera. We then use a golf pencil tied to the board with a fishing line to write.
Blue Brittle Star ©Am Ang Zhang 2010
So what about The NHS: A pencil solution?
Just copy Scotland; that “country” north of the border.
As much of the opposition to the new Bill is to do with the simple fact that it was a back handed way to privatise a major part of the NHS, the profitable part. Ordinary citizens without insurance will be left with a much depleted hospital service and those with insurance may find that over time they too might be dumped by their Private Health Insurers.
The Herald
JULIA HORTON
25 Feb 2009
Radical new legislation stopping private companies from running GP surgeries in Scotland is to be unveiled by ministers - further widening the divide between how the health service is run north and south of the border.
Explaining the purpose of the new legislation, which won near "unanimous" support from Scottish doctors during a recent consultation, Ms Sturgeon told The Herald: "We have decided to go ahead and legislate to effectively remove the possibility of commercial companies running GP practices.
"We want people providing GP services to be committed to the NHS and not to see it as a way of making a profit. I would hope that we would get considerable support for the bill from opposition MSPs."
The legislation, which ministers also expect to garner cross-party support, was sparked by concerns over a legal loophole which could allow into Scotland the kind of "creeping" privatisation of the NHS which is supported by the UK Government south of the border.
Trust in the government will return. There will not be any privatisation of primary or secondary care and that it would not go the way of the dental services.
Then those of us who could not afford private health care might be able to accept genuine and well thought out changes to the way the NHS will be run.
No more internal market, no more cherry picking and back to an integrated service.
By the way why not use the Scottish model that has now survived 10 years.
After devolution the NHS in England increased its reliance on a market-based approach – now one of the various controversies surrounding its future direction.
By contrast, NHS Scotland set about developing partnership agreements at national and board level as part of a strategy to engage staff in improving services.
The result, according to a study funded by the Economic and Social Research Council, is an “incredible common agenda” among interested parties from all quarters.
Research co-author Dr Peter Samuel said: “Although partnerships are found elsewhere in the public sector, NHS Scotland’s stands out as distinct and novel. It has survived for over a decade, defying reorganisation and changes in administrations, and it can offer valuable lessons in how to improve industrial relations.
By contrast, NHS Scotland set about developing partnership agreements at national and board level as part of a strategy to engage staff in improving services.
The result, according to a study funded by the Economic and Social Research Council, is an “incredible common agenda” among interested parties from all quarters.
Research co-author Dr Peter Samuel said: “Although partnerships are found elsewhere in the public sector, NHS Scotland’s stands out as distinct and novel. It has survived for over a decade, defying reorganisation and changes in administrations, and it can offer valuable lessons in how to improve industrial relations.
………Dr Samuel said: “The policymakers of NHS Scotland clearly concluded the only way to deliver better healthcare was to improve the way staff were engaged. This led to the establishment of various structures at national and local levels to give staff more say in decisions affecting their working lives and healthcare provision.
“NHS Scotland has even passed into law a ‘staff governance code’ that compels all its health boards to engage and involve staff and their representatives.
“This innovation in industrial relations is arguably one of the biggest examples of industrial democracy to be found anywhere in the world – and they have made it work.”
……….. We need to get back to using clinically relevant measures of performance that tell us how we are doing in comparison with our peers.
This has been repeatedly shown to be one of the most potent ways of modifying GP behaviour, and we should go back to it as a way of influencing clinical practice.
Scotland has no real truck with private medicine; APMS (Alternative Provider Medical Services) is not allowed. There is no market in healthcare as health boards keep primary and secondary care working together, and we actually speak to each other. Some of my best friends are consultants.
………… that trusting us to do our job is more effective than micromanagement.
Scotland: Serco NOT allowed to run GP practice
Friday, May 27, 2011
Quorum Sensing & E.Coli
As Germany
“Virulent bacteria do not want to begin secreting toxins too soon, or the host's immune system will quickly eliminate the nascent infection. Instead, Bassler explained, using quorum sensing, the bacteria count themselves and when they reach a sufficiently high number, they all launch their attack simultaneously. This way, the bacteria are more likely to overpower the immune system….” Bassler
……..many species of bacteria, including Escherichia coli MG1655, E. coli O157:H7, Salmonella typhimurium 14028, and S. typhimurium LT2 produce autoinducers similar or identical to the V. harveyi system 2 autoinducer AI-2. University of Calgary
Let us go back to an earlier post:
I am not a bacteriologist nor virologist but that did not stop me writing about these little creatures.
When I picked up the in-flight magazine on a recent flight, an article titled “Genius at Work” caught my eye. Bonnie Bassler is the bacteriologist at Princeton who discovered and pioneered the work on what she now called quorum sensing in microbes. To be more precise her initial work was with Vibrio harveyi. Vibrio is in the family of bacteria that causes Cholera. Vibrio vulnificus is carried by oysters and was most likely responsible for the serious illness of Michael Winner, film producer and now food writer of the London Sunday Times.
On following this up back home, I found an article on the website of Howard Hughes Medical Institute – she is one of the HHMI Investigators. From this article, I learned that:
“Virulent bacteria do not want to begin secreting toxins too soon, or the host's immune system will quickly eliminate the nascent infection. Instead, Bassler explained, using quorum sensing, the bacteria count themselves and when they reach a sufficiently high number, they all launch their attack simultaneously. This way, the bacteria are more likely to overpower the immune system….
For the past three hundred years……we’ve been completely wrong……we don’t know anything about bacteria until about a decade ago….”
Wow! Just as we thought we knew everything there is to know about microbes.
Bonnie Bassler will one day get the Nobel prize for medicine. You read it here first.
Fascinated, I wanted to find out more about this genius.
I would like to share with you her answers to some of questions that children were invited to ask about her life and work:
“You all asked me essentially the same question: how and when did I get interested in science. As a kid, I loved doing puzzles, solving riddles, and reading mystery books. I also loved animals and always had pets. Around high school, those interests (puzzle solving and animals) convinced me that I should be a veterinarian so I could work on mysterious illnesses in animals and cure them. In college, I realized I did not like big-bloody stuff. It became clear to me that I probably wouldn't enjoy being a vet, but I did not know what I'd do instead.
Fortunately, the vet curriculum required me to take biochemistry, genetics, and lab courses. Once I got into those classes, I fell in love with doing puzzles about little things (DNA and RNA and proteins and how they all fit together in cells). I also adored doing lab experiments and puzzling over my results. I realized that lab research was the perfect path for me. It allowed me to spend every day figuring out mysteries/puzzles that have to do with what make us alive. What could be a bigger mystery or puzzle? I changed my major in my junior year, and I have not left the lab since. (I still love animals and have a pet—Spark my cat—and I often go hiking hoping to see animals in the wild.)
I think being open-minded about what Nature is trying to tell you is the key to being creative and successful.”
Now in England
“The ability to dissect out a full set of cockroach salivary glands was a prerequisite requirement for medical school entrance in Hong Kong in our days. It is almost a 180 degree turn around nowadays when many young doctors have no idea about the biological world we live in. Nearly all Medical Schools in England
Related:
Cockroaches & Superbugs
Quorum Sensing: Cholera
NHS & Market Forces: Fund Holding & Medical Ethics
Dawn, anyone?
©Am Ang Zhang 2011
It was an interesting time during the brief few years of Fund Holding (FH). The idea that money should play no part in who gets seen was thrown out of the window. My hospital consultant colleagues all knew that preference will be given to referrals from Fund Holding practices. It was about survival. Less urgent cases would be seen if they come from FH practices.
Our Trust was small and we had to deal with two main FH practices and five non-FH ones. Child Psychiatry used to take self referrals but overnight that was stopped by our managers. Worryingly referrals from one FH practice dropped very dramatically. So the government’s clever idea may have some merit.
Then something strange happened. The other FH practice’s referrals shot up dramatically and this was across all disciplines.
Our managers thought: wow, more income for the Trust.
Not so the Cockroach Catcher and despite my protestation, I had to give their referrals preferential treatment.
“I thought it was based on clinical merit.”
Then, the bombshell: we were owed in excess of £2 million at the end of the second year and special administrator was sent in by the Authorities. We never got the extra money!
I quoted Prof. Waxman in an earlier post :
April 30, 2010 Jonathan Waxman
When I started in medicine, the hospital was run by about three people. Things were so much more simple when doctors and nurses treated patients, doing their best without the guidance of guidelines and targets, doing their best ... yes ... to make the patients better. How did we manage without forms to fill and waiting times compliance? Quite well actually. The medical director ran the medical side of things while matron and the accountant handled the rest. It wasn’t much of a business then: it didn’t have to be, because there was no internal market to manage.
The internal market’s billing system is not only costly and bureaucratic, the theory that underpins it is absurd. Why should a bill for the treatment of a patient go out to Oldham or Oxford, when it is not Oldham or Oxford that pays the bill — there is only one person that picks up the tab: the taxpayer, you and me.
And there are big problems with the billing process. For example, if a patient is seen in an outpatient clinic then there is a charge made by the hospital for his or her first attendance — but follow-up appointments are not charged. And if many treatments are given in a hospital to a patient, only the most expensive of the treatment episodes is charged.
250,000 administrative staff
There are savings to be made. It is alleged that there are just 75,000 administrators at work in the NHS but this figure is laughably mythological.
One report by the Centre for Policy Studies published in 2003 indicated that there were 250,000 administrative staff employed in the NHS: at least one administrator for every nurse.
Disempowerment
There is a general feeling in the NHS of disempowerment of the professionals. People can’t face up to the incredible struggle, the disapproval that faces any of them if they have the temerity to suggest that things should be run differently.
The principle of care for all from cradle to grave is worthy and wonderful. But the current reality is a cradle rocked by accountants who are incapable of even counting the number of times that they have rocked it. The reality is gravediggers working with a cost improvement shovel made of rust.
The Nation as a whole
Moving patients from one place to another does not save the nation’s money, though it might save a local hospital some dosh. So the internal market has failed because it does not consider the health of the nation as a whole, merely the finances of a single hospital department, a local hospital or GP practice.
So what should we do? Let us go back to the old discipline of the NHS. Let the professionals manage medicine, empower the professionals, the doctors and nurses and shove the internal market in the bin and screw down the lid. At this election time please let us hear from all political parties that they will ditch this absurd love-affair with the internal market. Instead let them help the NHS do what it does best — treat patients, and do so efficiently and economically without the crucifying expense and ridiculous parody of competition.
Why should anyone worry who provides healthcare? Because the weight of evidence is that private markets in health bring exorbitant administrative costs, lead to cherrypicking of more profitable patients, increase inequity and the postcode lottery gap, generate conflicts of interest, are unaccountable, and increase pressure for top-up payments and "care package" limits.
Keith Palmer on competition and choice
“…….competition and choice in contestable services may inadvertently cause deterioration in the quality of essential services provided by financially challenged trusts, and therefore widen the quality gap between the best and worst performers. Market forces alone will rarely drive trusts into voluntary agreement to reconfigure in ways that will improve quality and reduce costs. In most cases, the most likely outcome is that financially challenged trusts will suffer a downward spiral of continuing financial deficits, deterioration in the quality of care and a further widening of the quality gap. The NHS will have no alternative but to continue to fund these deficits or allow the trusts to fail.” RECONFIGURING HOSPITAL SERVICES: Lessons from South East London
NHS & Monitor: Toyota & McKinsey
Thursday, May 26, 2011
Wine & Tea: NHS Privatisation
As the NHS reform bill faced a delay of six months thanks to Nick Clegg, it looks like the privateers will have to wait a while longer.
Will the NHS really be privatised?
This is not the view of The Cockroach Catcher.
As he dined with his good friend who served a beautifully fresh Red Mullet cooked the Chinese style with a simple spring onion sauce, the Cockroach Catcher produced a bottle of his recent discovery: Torrontes from Argentina.
Torrontes is truly an Argentinian wine that is really suitable for our Chinese Style of cooking. On the nose, it has a delicate pear and citrus flavour. My friend who is used to the good and expensive wines took a sip and declared that it has a wonderful peach flavour. It has a long aftertaste that is unusual for this class of wine. At the price, it beats any other white wine. Let us keep that as a secret.
Over tea afterwards the topic of NHS privatization came up.
No, not all of NHS will be privatized.
Why?
And some us pay taxes!!!
So nobody in their right mind would want to privatise the NHS. There is certainly more money to be made if it remained in the public domain.
Dave Cameron’s brother-in-law should not worry either as his income would go up at least 300% as long as he works for one of the private providers.
Business is business!!!
But the sums are somehow wrong!
If the private providers are making money and the GP commissioning teams have a limited pot and that Consultants working for the likes of BMI hospitals have a 300% increase in pay compared to old NHS Hospital pay scale, either tax payers are going to be forking out more and more money or someone is not going to get their treatment.
Is some politician heading for a top job with the likes of GHG or Bupa? Only time will tell and history told us it won’t be long: less than 2 years.
Will the NHS really be privatised?
This is not the view of The Cockroach Catcher.
As he dined with his good friend who served a beautifully fresh Red Mullet cooked the Chinese style with a simple spring onion sauce, the Cockroach Catcher produced a bottle of his recent discovery: Torrontes from Argentina.
Torrontes is truly an Argentinian wine that is really suitable for our Chinese Style of cooking. On the nose, it has a delicate pear and citrus flavour. My friend who is used to the good and expensive wines took a sip and declared that it has a wonderful peach flavour. It has a long aftertaste that is unusual for this class of wine. At the price, it beats any other white wine. Let us keep that as a secret.
Over tea afterwards the topic of NHS privatization came up.
No, not all of NHS will be privatized.
Why?
Government money is the best money for anyone to make and that is really tax payer’s money. The new NHS will be the private sector’s main source of income, as only 90,000 in the UK are covered by private insurance and often they are offered cash incentives to use the NHS.
It is therefore essential for the private health care companies that the NHS is around, at least in name, so that they can make money by providing a “better value and more competitive” service to the NHS!
Some parts of the NHS will have to remain too, as it is necessary for the private sector to dump the un-profitable patients: the chronic and the long term mentally ill, for example. (Right now, 25% of NHS psychiatric patients are treated by the private sector. But why? Even in psychiatry, there are cherries to be picked.)
Finally, in order to keep the mortality figures low at competing private hospitals, they need to be able to rush some of their patients off to NHS hospitals at the critical moments!
Have some more tea!!!
Iron Goddess of Mercy (Oolong Tea ): traditional tea of my friend's home village, Teochiu which is of course where my family is from.
These are traditional tiny cups and the tea is lovely on the nose and has a long aftertaste. To do this tea justice, use the softest water you can get: like those for a good malt!!! (Calcium is the villain here: no more than 12mg/Litre)
So the NHS will be free at the point of delivery.
Lets hope so but the money must come from somewhere.And some us pay taxes!!!
So nobody in their right mind would want to privatise the NHS. There is certainly more money to be made if it remained in the public domain.
Dave Cameron’s brother-in-law should not worry either as his income would go up at least 300% as long as he works for one of the private providers.
Business is business!!!
But the sums are somehow wrong!
If the private providers are making money and the GP commissioning teams have a limited pot and that Consultants working for the likes of BMI hospitals have a 300% increase in pay compared to old NHS Hospital pay scale, either tax payers are going to be forking out more and more money or someone is not going to get their treatment.
Is some politician heading for a top job with the likes of GHG or Bupa? Only time will tell and history told us it won’t be long: less than 2 years.
Wine Posts:
Related:
Tuesday, May 24, 2011
NHS 1978: Hope, Faith & Supermarket
It is well known that we as doctors do not have all the answers and we can only base our diagnosis and treatment on current knowledge.
Patients or their relatives are used to trust the judgement of doctors and always hope for a better or even miraculous outcome. Their faith in their doctor is often supplemented by their own religious faith.
David Cameron is no different and he has stated so on record.
I am not here to analyse his faith.
I am here to re-tell one of the stories of hope and faith I have experienced as a very junior consultant in 1978
The Mayo of the
The year was 1978 and I was employed by one of the fourteen Regional Health Authorities. The perceived wisdom was to allow consultants freedom from Area and District control that may not be of benefit to the NHS as a whole so the local Area or District Health did not hold our contracts. Even for matters like Annual Leave and Study Leave we dealt directly with RHA.
Referrals were accepted from GPs and we could refer to other specialists within the Region or to the any of the major London Centres of excellence. Many of us were trained by some of these centres and we respected them. They were the Mayos and Clevelands and Hopkins of the United Kingdom
Money or funding never came into it and we truly had a most integrated service.
We used to practice real, good and economical medicine.
We used to practice real, good and economical medicine.
The unusual cases:
Child Psychiatry like many other disciplines in medicine does not follow rules and do not function like supermarkets. Supermarkets have very advanced systems to track customer demands and they can maximise profit and keep cost down. In medicine we do sometimes get unusual cases that would have been a nightmare for the supermarket trained managers.
As it is so difficult to plan for the unusual it will become even more difficult if the present government had its way (and there is every sign that they will), not only will the reformed NHS find it difficult to cope with the unusual, it will find it extremely difficult to cope with emergencies.
Supermarket:
Why? These cases cost money and in the new world of Supermarket Styled NHS, they have to be dealt with! For that reason, not all NHS hospitals will be failed by Monitor. Some will need to be kept in order that someone could then deal with unprofitable cases. They will be the new fall guys.
But supermarkets can get things wrong too. In Spain
©Am Ang Zhang 2010
Back to the patient:
Would my patient be dealt with in the same way in 2011?
GP to Paediatrician: 13 year old with one stiff arm. Seen the same day.
Paediatrician to me: ? Psychosis or even Catatonia.
Seen same day and admitted to Paediatric Ward, DGH.
Child Psychiatrist to Gynaecologist: ? Pregnancy or tumour. Still the same day.
Gynaecologist to Radiologist: Unlikely to be pregnant, ? Ovarian cyst.
Radiologist (Hospital & no India
Gynaecologist: Operation on emergency basis with Paediatric Anaethetics Consultant. Still Day 1.
Patient unconscious and transferred to GOS on same day. Seen by various Professors.
Patient later transferred to Queen’s Square (National Hospital
Seen by more Professors.
Regained consciousness after 23 days.
Eventually transferred back to local Hospital.
None of the Doctor to Doctor decisions need to be referred to managers.
We did not have Admission Avoidance then.
How is the new Consortia going to work out the funding and how are the three Foundation Trust Hospitals going to work out the costs.
The danger is that the patient may not even get to see the first Specialist: Paediatrician not to say the second one: me.
Not to mention the operation etc. and the transfer to the Centres of excellence.
Here is an extract from my book The Cockroach Catcher: Chapter 29 The Power of Prayers
…………Something else was going on here, and I was not happy because I did not know what it was. I was supposed to know and I generally did. After all I was the consultant now.
Thank goodness she could breathe without assistance. That was the first thing I noticed. I saw mother in the corner obviously in tears. She asked if her daughter would be all right. I cannot remember what I said but knowing myself I could not have said anything too discouraging. But then I knew I was in tricky territory and it was unlikely to be the territory of a child psychiatrist.
A good doctor is one who is not afraid to ask for help but he must also know where to ask.
“Get me Great Ormond Street
“I already did.”
She is going to be a good doctor.
“Well, the Regional unit said that they had no beds so I thought I should ring up my classmate at GOS and she talked to her SR who said “send her in”.”
Who needs consultants when juniors have that kind of network? This girl will do well.
“Everything has been set up. The ambulance will be here in about half an hour and if it is all right I would like to go with her.”
“Yes, you do and thanks a lot.”
I told mother that we were transferring her daughter to the best children’s hospital inEngland
“........Ten years later mother came to see my secretary and left a photo. It was a photo of her daughter and her new baby. She had been working at the local bank since she left school, met a very nice man and now she had a baby. Mother thought I might remember them and perhaps I would be pleased with the outcome.
"I was very pleased for them too but I would hate for anyone to put faith or god to such a test too often."
David Cameron, if it was your plan not to have an integrated service, then there is not much we ordinary people could do except pray. If it was not your intention, then could you let us have an integrated service! That way you would not need many accountants and you will save money in doing so.
Just like Mayo Clinic:
“…….Mayo offers proof that when a like-minded group of doctors practice medicine to the very best of their ability—without worrying about the revenues they are bringing in for the hospital, the fees they are accumulating for themselves, or even whether the patient can pay—patients satisfaction is higher, physicians are happier, and the medical bills are lower.”
But it is probably too late:
Just like Mayo Clinic:
“…….Mayo offers proof that when a like-minded group of doctors practice medicine to the very best of their ability—without worrying about the revenues they are bringing in for the hospital, the fees they are accumulating for themselves, or even whether the patient can pay—patients satisfaction is higher, physicians are happier, and the medical bills are lower.”
But it is probably too late:
Pulse: GP consortium chairs are overwhelmingly opposed to any requirement to include hospital consultants on their boards, viewing it as a serious conflict of interest that would undermine the commissioning process, finds a Pulse survey.
King’s Fund: Million £ GP.
See also:























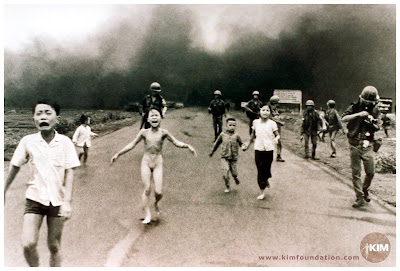 “By rights possibly one of the most damaged psychologically and physically. She underwent no fewer than seventeen operations. The photo of her running down the street of Saigon naked probably changed the course of the Vietnam War and the world’s perception of good and bad. Then came her dramatic escape in 1992 to Newfoundland and her eventual settling down in Canada. Human resilience is not to be underestimated and the imposition of psychological intervention could represent a great under-estimation of our genetical endowment. At one of her public lectures, one of the war veterans who was a helicopter gunner broke down.”
“By rights possibly one of the most damaged psychologically and physically. She underwent no fewer than seventeen operations. The photo of her running down the street of Saigon naked probably changed the course of the Vietnam War and the world’s perception of good and bad. Then came her dramatic escape in 1992 to Newfoundland and her eventual settling down in Canada. Human resilience is not to be underestimated and the imposition of psychological intervention could represent a great under-estimation of our genetical endowment. At one of her public lectures, one of the war veterans who was a helicopter gunner broke down.”